Rev Bras Fisiol Exerc.
2024;23(3):e235611
ORIGINAL ARTICLE
Physiological changes associated with virtual reality in patients
undergoing coronary artery bypass grafting
Alterações
fisiológicas associadas à realidade virtual em pacientes submetidos à cirurgia
de revascularização do miocárdio
André Luiz Lisboa Cordeiro¹,2,
Gleisiane de Oliveira Santos¹, Késsia
Morgana Vital Oliveira¹, Nathaly Carneiro da Silva¹,
Rafaela da Silva Sales¹, André Raimundo Guimarães3
1Escola Bahiana de Medicina e Saúde
Pública, Salvador, BA, Brazil
2Centre Universitário Nobre, Feira de
Santana, Bahia, Brazil
3Instituto Nobre de Cardiologia, Feira de
Santana, Bahia, Brazil
Received: November 28,
2024; Accepted: December
15, 2024.
Correspondence: André Luiz Lisboa Cordeiro, andrelisboacordeiro@gmail.com
How to cite
Cordeiro ALL, Santos GO,
Oliveira KMV, Silva NC, Sales RS, Guimarães AR. Physiological changes
associated with virtual reality in patients undergoing coronary artery bypass
grafting. Rev Bras Fisiol Exerc. 2024;23(3):e235611. doi:
10.33233/rbfex.v23i3.5611
Abstract
Introduction: Coronary Artery Bypass Grafting (CABG) promotes
physiological changes in patients, and Virtual Reality (VR) is an option within
the cardiac rehabilitation program that may help them reduce discomfort and
control physiological parameters. Objective: To describe the
physiological changes caused by the practice of VR in patients undergoing CABG.
Methods: Cross-sectional study. Patients undergoing CABG used VR using
the XBOX 360 device plus Kinect from the third day after cardiac surgery.
Systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR),
respiratory rate (RF), oxygen saturation (SaO2) and temperature were assessed
on three occasions: before VR application, at the end of the session and one
hour after recovery. Results: 31 patients were included, with a mean age
of 54 ± 8 years, with a higher prevalence in males with 21 (68%) individuals.
The SBP was 123 mmHg ± 18 at baseline, 133 mmHg ± 17 (p = 0.25) immediately
after the intervention, and 121mmHg ± 15 (p = 0.43) at recovery. The HR
variable was analyzed in the pre-test with 81 bpm ± 11, in the post-test 92 bpm
± 12 (p = 0.32), and in the recovery 83 bpm ± 13 (p = 0.83). SpO2
was found in the pre-test 96% ± 1, in the post-test 96% ± 1 (p = 0.83), and in
the recovery 97% ± 2 (p = 0.84). Comparing the variables of the pre with
post-test and this with those of recovery, despite the clinical changes, they
did not show statistical significance. Conclusion: The physiological
parameters evaluated, despite the variations, showed that their applicability
to virtual reality is safe and viable.
Keywords: monitoring, physiologic; thoracic surgery; virtual
reality; early ambulation
Resumo
Introdução: A cirurgia de revascularização do
miocárdio (CRM) promove alterações fisiológicas nos pacientes e a Realidade
Virtual (RV) é uma opção dentro do programa de reabilitação cardíaca, que pode
ajudar a reduzir o desconforto e controlar os parâmetros fisiológicos. Objetivo:
Descrever as alterações fisiológicas causadas pela prática da RV em pacientes
submetidos à CRM. Métodos: Estudo transversal. Os pacientes submetidos à
CRM utilizaram a RV por meio do aparelho XBOX 360
mais Kinect a partir do terceiro dia após a cirurgia cardíaca. A pressão
arterial sistólica (PAS), a pressão arterial diastólica (PAD), a frequência
cardíaca (FC), a frequência respiratória (FR), a saturação de oxigênio (SaO2)
e a temperatura foram avaliadas em três momentos: antes da aplicação da RV,
após o término da sessão e uma hora após a recuperação. Resultados:
Foram incluídos 31 pacientes, com média de idade de 54 ± 8 anos, com maior
prevalência no sexo masculino com 21 (68%) indivíduos. A PAS foi inicialmente
de 123 mmHg ± 18, 133 mmHg ± 17 (p = 0,25) imediatamente após a intervenção e
121 mmHg ± 15 (p = 0,43) na recuperação. A variável FC foi analisada no
pré-teste com 81 bpm ± 11, no pós-teste com 92 bpm ± 12 (p = 0,32), e na
recuperação com 83 bpm ± 13 (p = 0,83). A SpO2 foi encontrada no pré com 96% ± 1, no pós-teste com 96% ± 1 (p = 0,83), e na
recuperação com 97% ± 2 (p = 0,84). Comparando as variáveis do pré com o pós-teste e deste com as da recuperação, apesar
das alterações clínicas, não se verificou uma diferença estatisticamente
significativa. Conclusão: Os parâmetros fisiológicos avaliados, apesar
das variações, mostraram que a sua aplicabilidade à realidade virtual é segura
e viável.
Palavras-chave: monitoramento fisiológico; cirurgia
cardíaca; realidade virtual; deambulação precoce
Introduction
Cardiovascular disease is one of the main causes of
morbidity and mortality in the world, and cardiac rehabilitation is a measure
to reduce and/or prevent the progression of cardiovascular disease in
approximately 50% of patients undergoing cardiac surgery. There is an
association between patients affected by cardiovascular diseases and the
occurrence of other complications such as functional dependence, which impacts
on the quality of life of these patients [1,2].
The increasing average age of patients undergoing cardiac
surgery (CS) and the consequent increase in the number of procedures performed,
with myocardial revascularization being the most common, has led to a need for
updating by healthcare professionals to improve the quality of life and
increase the survival of these patients [3]. Thus, based on the literature,
there are several complications commonly associated with this surgical
intervention, which brings the need to update these professionals about them
[4]
Cardiac surgery is a highly complex procedure that
promotes physiological changes usually induced by anesthesia, extracorporeal
circulation and cardioplegia, the effects of which can last until the
postoperative period, with several complications such as hemodynamic
instability [5]. The critical patient, during hospitalization in the Intensive
Care Unit (ICU), lives with several factors that cause stress and,
consequently, generate cognitive changes, respiratory rate, heart rate and
blood pressure [6].
Virtual Reality (VR) is a resource that, when
implemented, especially in ICU patients undergoing cardiac surgery, can favor
the reduction of discomfort and physiological parameters, as a way to inhibit
pain due to exposure to noise and stress psychological impact of this
environment, which causes overload in the individual's functional capacity and
long-term cognitive impairment [6]. When increasing the visual stimulus,
strategies are used to distract the critical patient's attention and,
consequently, the experience of the mental process of pain, causing an increase
in temperature, a decrease in heart rate, respiratory rate and the intensity of
chronic pain, which indicates relaxation through distraction during the
acquisition of virtual technologies [7].
A recent study that added VR to a Cardiac Rehabilitation
(CR) program showed that the hemodynamic responses in some variables were more
intense than in conventional CR. Nevertheless, the values are similar, thus
suggesting a new strategy that can be used in CR, and with the necessary care,
such as: selection of stable patients, intensification of monitoring for better
control and, whenever necessary, correction of the movement performed by the
patient [8].
The physiological responses observed with the greatest
intensity when using VR were heart rate, respiratory rate and maintenance of
effort during activity and five minutes after application of the intervention
[8]. Therefore, the present study aims to describe the physiological changes
generated with the practice of VR in patients undergoing coronary artery bypass
grafting (CABG).
Methods
This cross-sectional study was carried out with patients
undergoing cardiac surgery at the Instituto Nobre de Cardiologia (incardio) in
Feira de Santana, Bahia. The study was approved by the Research Ethics
Committee of Faculdade Nobre under number 2,150,434. All volunteers signed a
Free and Informed Consent Form.
Eligibility criteria
Individuals of both sexes, aged over 18 years, who signed
the Free and Informed Consent Form (ICF) and underwent cardiac myocardial
revascularization (MR) surgery, via median sternotomy and cardiopulmonary
bypass, were included. Individuals with hemodynamic instability, before
starting or during exercise, with Mean Arterial Pressure (MAP) (< 70 mmHg or
> 110 mmHg), hypotension or hypertension, drop in oxygen saturation (<
90%), arrhythmias before or during the game, tachycardia (> 100 beats per
minute), bradycardia (< 60 beats per minute), tachypnea (> 20 breaths per
minute) and bradypnea (<12 breaths per minute) were excluded. Also excluded
were those with angina or dyspnea at rest, inability to perform the proposed
techniques (physical limitations and/or psychological alteration), withdrawal
during the practice of the virtual reality protocol, reintubation, time in the
Intensive Care Unit greater than three days, time of mechanical ventilation
above 24 hours and proven pneumopathy.
Study protocol
On the third day after heart surgery, all vital signs,
such as Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Heart
Rate (HR), Respiratory Rate (RF), Oxygen Saturation (SaO2) and
temperature were evaluated before applying VR.
VR was performed with the XBOX 360 platform added to the
Kinect electronic device. The game used was the Kinect Sports Ultimate
Collection, Table Tennis mode. The orthostatic patient, facing the TV, with 20
minutes of daily game practice time, performed functional movements such as:
elbow flexion-extension, internal and external rotation of the upper limbs as
well as adduction and abduction, hip dissociation and weight loss in the lower
limbs. After the game, patients had their vital signs checked again, with the
same procedure repeated one hour after recovery.
SBP and DBP were assessed with the patient under sedation
using a stethoscope (Littmann, Saint Paul, USA) and an aneroid sphygmomanometer
(Welch Allyn-Tycos, New York, USA). HR was obtained using a validated heart
rate monitor (Polar RS800CX, Polar Electro, Kempele, Finland). The RR was
measured by counting the respiratory incursions per minute without the
patient’s knowledge of the procedure, so that the usual ventilation is not
modified. SpO2 was assessed using
a pulse oximeter (Mindray
PM-50 Pulse Oximeter, China). The temperature
was assessed with a Digital Clinical Thermometer
(Incoterm Termo Med).
Data analysis
For data analysis, the Statistical Package for Social
Sciences (SPSS) version 20.0 was used. To assess the normality of the sample,
the Shapiro Wilks Test was used. Categorical variables were assessed using the
Chi-square. The comparison of numerical variables between groups was performed
using the independent Student's T Test. It was considered significant when p
< 0.05.
Results
The sample of this study consisted of 76 patients who
underwent cardiac surgery and were admitted to the Inpatient Unit (IU), after
the procedure and discharge from the Intensive Care Unit (ICU), from August
2017 to April 2018. 45 patients were excluded from the study, according to the
exclusion criteria, leaving 31 patients who met the inclusion criteria of the
study.
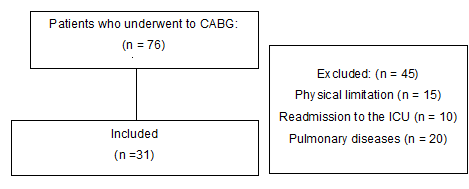
Figure 1 - Flowchart of inclusion of patients in the study
We included 31 patients, with a mean age of 54 ± 8 years,
with a higher prevalence in males with 21 (68%) individuals. The most common
comorbidities were sedentary lifestyle in 20 (65%) patients and SAH in 18 (58%)
patients. Table I presents the clinical characteristics of the patients
included in the study.
Table I - Clinical characteristics of patients included in
the study
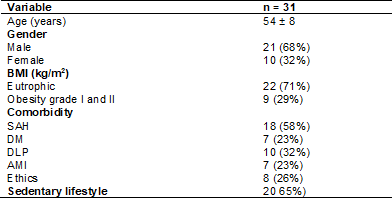
BMI = Body Mass Index; SAH = Systemic Arterial
Hypertension; DM = Diabetes Mellitus; DLP = Dyslipidemia; AMI = Acute
Myocardial Infarction
Table II describes the surgical characteristics of the
patients included in the study. The mean time of cardiopulmonary bypass found
in our study was 63 ± 22 minutes and mechanical ventilation found 7 ± 3 hours.
Table II - Surgical characteristics of the patients included in
the study
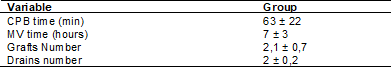
CPB = Cardiopulmonary bypass; MV = Mechanical Ventilation
Table III shows the behavior of cardiovascular and
respiratory variables at different times of the study. The SBP was 123 mmHg ±
18 at baseline, 133 mmHg ± 17 (p = 0.25) immediately after intervention, and
121 mmHg ± 15 (p = 0.43) during recovery. The HR variable was analyzed in the
pre-test with 81 bpm ± 11 and in the post-test with 92 bpm ± 12 (p = 0.32),
being verified in the recovery with 83 bpm ± 13 (p = 0.83). SpO2 was found in
the pre-test 96% ± 1 and in the post-test the same result 96% ± 1 (p = 0.83),
and in the recovery period with 97% ± 2 (p = 0.84). Comparing the variables of
the pre-test with those of the post-test and this with those of recovery,
despite the clinical changes, did not show statistical significance.
Table III - Behavior of cardiovascular and respiratory
variables at different times of the study
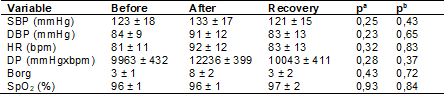
aComparison between the
pre-test and the post-test; bComparison of the pre-test for
recovery; SBP = Systolic Blood Pressure; DBP = Diastolic Blood Pressure; HR =
Heart rate; DP = Double Product; SpO2 = Peripheral Oxygen Saturation
Discussion
In the present study, it was possible to verify that
there was no change in the physiological variables evaluated in patients who
performed exercises through VR in the postoperative period compared to the
preoperative period in patients who underwent coronary artery bypass surgery,
which represents safety.
Studies have shown that surgical
intervention associated with risk factors leads to changes throughout the body.
Cardiac surgeries are usually performed through a sternotomy, an extensive and
traumatic incision that causes chest instability [9], resulting in shallow
breathing, difficulty in gas exchange, and predisposition to pulmonary changes
[10], in addition, it is very common in patients to experience pain, limiting
movements and bed positioning [11].
Immobility causes respiratory [12], neuromuscular,
cardiovascular, cognitive and quality-of-life complications, and can persist
for up to five years after hospital discharge [13]. Patients who develop
postoperative complications spend more time in the ICU and in the hospital,
resulting in increased healthcare costs and reduced quality of life [14,15]. In
addition, it is common for patients to experience a melancholic state, with
symptoms of anxiety, apprehension, worry and depression, impairing psychological
and physiological recovery [16].
Yayla and Özer [17] highlighted the importance of early
mobilization in the ICU and in the cardiac surgical clinic, reducing
postoperative complications, length of hospital stay and improving sleep
quality, confirming Ribeiro et al. [18], who also found an improvement
in autonomic modulation. Early mobilization optimizes functionality, reduces
the duration of mechanical ventilation, and provides psychological benefits,
being considered the gold standard in cardiopulmonary dysfunctions [19]. From
this perspective, they saw the need for a motivational strategy that could
assist in the patient’s recovery, thus initiating the use of VR as a strategy
for cardiac rehabilitation [20].
VR is an intervention that, in addition to being well
accepted, immersive, easy to apply [6], with punctuation feedback and mixed
reality [21], studies have shown that VR causes relaxation by reducing
psychophysiological stress [16], pain [22], anxiety [7], improves mood [23],
restores cognitive and attention capacities [2], can be a promising and
low-cost pharmacological intervention to prevent delirium and reduce the use of
analgesics [22]. They can be used as a treatment method for balance, postural control,
and rehabilitation of body segments [24]. Cacau et al. [20] demonstrated
improved mobility in patients undergoing cardiac surgery, resulting in faster
recovery and earlier hospital discharge.
In a study by Cruz et al. [8], in which they
sought to verify the acute hemodynamic effects of adding VR using exergames for
patients undergoing cardiac rehabilitation, they showed that VR produced a
similar physiological pattern of acute hemodynamic effects in CR. However, there
was a greater significance in HR, RR and perceived effort rate during VR and
for up to five minutes after the session. Although the effects were greater,
they were within the expected normal standards and the VR promoted enough
intensity for the patients to reach their heart rate reserve. These results
corroborate similar findings in our study, in which it was found that, despite
the clinical changes, the physiological variables of the patients who underwent
virtual reality did not show statistical significance when comparing the
pre-test with the post-test, ensuring that the use of VR does not harm the
patient's recovery.
Ribeiro et al. [18], in a study, analyzed
different physiotherapy protocols in heart rate variability in patients
undergoing CABG and observed in the virtual reality group that motor
physiotherapy associated with VR activities was more effective, resulting in
improved heart rate modulation and reduced hospital stay in this population,
while in the control group it showed a worse cardiac autonomic response and no
reduction in oxygen saturation, hypotension or arterial hypertension, syncope
or arrhythmia was observed during the application of the protocols. For Masroor
et al. [25], this fact may be associated with an increase in
parasympathetic stimulation together with a decrease in the effect of
adrenergic stimulation on the heart, thus reducing heart rate at rest and
benefiting patients with cardiovascular disease in performing the activity.
In the study carried out by Rodrigues et al. [26],
an improvement in the cardiorespiratory capacity of the participants was
demonstrated, and the group that used virtual reality reached the
pre-determined goals in a shorter time, when compared to the control group.
This aspect was also confirmed in our study, showing that virtual reality is
safe, since there was no significant change during or after the realization.
However, it is worth mentioning that some precautions must be considered, such
as greater monitoring of cardiovascular parameters to control the intensity.
As limitations, our study presented a reduced sample size
and number of sessions, a lack of assessment of intensity and motivation and
patient satisfaction.
Conclusion
Based on the results, it was found that the virtual
reality intervention in the postoperative period of cardiac rehabilitation
promotes physiological responses within normal standards and is a safe and
viable intervention in this patient profile.
Conflict of interest
The authors reported no conflict of interest
Sources of funding
There were
no external sources of funding for this study
Author’s contribution
Conception and
design of the research: Cordeiro ALL; Data collection:
Santos GO, Oliveira KMV, Silva NC, Sales RS; Data analysis
and interpretation:
Cordeiro ALL; Statistical analysis:
Cordeiro ALL; Manuscript writing: Santos GO, Oliveira KMV, Silva NC, Sales RS; Critical revision of the manuscript
for important intellectual content: Cordeiro ALL, Guimarães AR
References
- García-Bravo S, Cuesta-Gómez A, Campuzano-Ruiz R, López-Navas MJ,
Domínguez-Paniagua J, Araújo-Narváez A, et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil Rehabil.
2021;43(4):448-57. doi: 10.1080/09638288.2019.1631892 [Crossref]
- Vieira A, Melo C, Machado J, Gabriel J. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: a randomized controlled trial. Disabil Rehabil Assist Technol. 2017;13(2):112-23. doi: 10.1080/17483107.2017.1297858 [Crossref]
- Cielo C, Silveira M, Arboit EL, Camponogara S. Expectations of patients submitted to myocardial revascularization surgery at the time of hospital discharge. J Res.: Fundam Care. Online. 2015;7(3): 2670-87. doi: 10.9789/2175-5361.2015.v7i3.2670-2687 [Crossref]
- Cordeiro ALL, Brito AAOR, Santana NMA, Silva INMS, Nogueira SCO, Guimarães ARF, et al. Análise do grau de independência funcional pré e na alta da uti em pacientes submetidos à cirurgia cardíaca. Rev Pesqui Fisioter. 2015;5(1):21-27. doi: 10.17267/2238-2704rpf.v5i1.574 [Crossref]
- Kaufmann J, Kung E. Factors affecting cardiovascular physiology in cardiothoracic surgery: implications for lumped-parameter modeling. Front Surg. 2019;6(62):1-7. doi: 10.3389/fsurg.2019.00062 [Crossref]
- Gerber SM, Jeitziner MM, Knobel SEJ, Mosimann UP, Müri RM, Jakob SM, et al. Perception and performance on a virtual reality cognitive stimulation for use in the intensive care unit: a non-randomized trial in critically Ill patients. Front Med. 2019; 6(287):1-9. doi: 10.3389/fmed.2019.00287 [Crossref]
- Wiederhold BK, Gao K, Sulea C, Wiederhold, MD. Virtual reality as a distraction technique in chronic pain patients. Cyberpsychol Behav Soc Netw. 2014;17(6):346-52. doi: 10.1089/cyber.2014.0207 [Crossref]
- Cruz MMA, Ricci-Vitor AL, Borges GLB, Silva PF, Ribeiro F, Vanderlei LCM. Acute hemodynamic effects of virtual reality based-therapy in patients of cardiovascular rehabilitation: cluster randomized crossover trial. Arch Phys Med Rehabil. 2020;101(4): 642-9. doi: 10.1016/j.apmr.2019.12.006 [Crossref]
- Giacomazzi CM, Lagni VB, Monteiro MB. Postoperative pain as a contributor to pulmonary function impairment in patients submitted to heart surgery. Braz J Cardiovasc Surg. 2006;21(4):386-392. doi: 10.1590/S0102-76382006000400008 [Crossref]
- Sasseron AB, Figueiredo LC, Trova K, Cardoso AL, Lima NMFV, Olmos SC, et al. Does the pain disturb the respiratory function after heart surgeries? Rev Bras Cir Cardiovasc. 2009;24(4):490-6. doi: 10.1590/s0102-76382009000500010 [Crossref]
- Laizo A, Delgado FEF, Rocha GM. Complications that increase the time of Hospitalization at ICU of patients submitted to cardiac surgery. Rev Bras Cir Cardiovasc. 2010;25(2):166-71. doi: 10.1590/S0102-76382010000200007 [Crossref]
- Cavayas YA, Eljaiek R, Rodrigue E, Lamarche Y, Girard M, Wang HT, et al. Preoperative diaphragm function is associated with postoperative pulmonary complications after cardiac surgery. Crit Care Med. 2019;47(12):e966-e974. doi: 10.1097/CCM.0000000000004027 [Crossref]
- Burtin C, Clerckx B, Robbeets C, Ferdinande P, Langer D, Troosters T, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009;37(9):2499-505. doi: 10.1097/CCM.0b013e3181a38937 [Crossref]
- Oliveira EK, Silva VZM, Turquetto ALR. Relationship of postoperative walk
test and lung function with the length of heart surgery hospital stay. Rev Bras Cir Cardiovasc.
2009;24(4):478-484. doi: 10.1590/s0102-76382009000500008 [Crossref]
- Steffens E, Dallazen F, Santori C, Chiapinotto S, Battisti IDE, Winkelmann ER. Physical and functional conditions and quality of life in patients in pre and post-operative cardiac surgery. Rev Pesqui Fisioter. 2016;6(4):422-9. doi: 10.17267/2238-2704rpf.v6i4.1149 [Crossref]
- Mosso-Vázquez JL, Gao K, Wiederhold BK, Wiederhold MD. Virtual reality for pain management in cardiac surgery. Cyberpsychol Behav Soc Netw. 2014; 17(6):371-8. doi: 10.1089/cyber.2014.0198 [Crossref]
- Yayla A, Özer N. Effects of early mobilization protocol performed after cardiac surgery on patient care outcomes. Int J Nurs Pract. 2019;25(6):e12784. doi: 10.1111/ijn.12784 [Crossref]
- Ribeiro BC, Poça JJG, Rocha
AMC, Cunha CNS, Cunha KC, Falcão LFM, et al. Different
physiotherapy protocols after coronary artery bypass graft surgery: A
randomized controlled trial. Physiother Res Int. 2020; e1882. doi: 10.1002/pri.1882 [Crossref]
- Gosselink R, Bott J, Johnson M, Dean E, Nava S, Norrenberg M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008;34(7):1188-99. doi: 10.1007/s00134-008-1026-7 [Crossref]
- Cacau LAP, Oliveira GU, Maynard LG, Araújo Filho AA, Silva Júnior WM, Cerqueira Neto ML, et al. The use of the virtual reality as intervention tool in the postoperative of cardiac surgery. Rev Bras Cir Cardiovasc. 2013;28(2):281-9. doi: 10.5935/1678-9741.20130039 [Crossref]
- Wiederhold MD, Crisci M, Patel V, Nonaka M, Wiederhold BK. Physiological monitoring during augmented reality exercise confirms advantages to health and well-being. Cyberpsychol Behav Soc Netw. 2019;22(2): 122-126. doi: 10.1089/cyber.2018.0027 [Crossref]
- Freitas DMO, Spadoni VS. A realidade virtual é útil para manejo da dor em pacientes submetidos a procedimentos médicos? Einstein. 2019;17(2):eMD4837. doi: 10.31744/einstein_journal/2019MD4837 [Crossref]
- Kamińska D, Smółka K, Zwoliński G, Wiak S, Merecz-Kot D, Anbarjafari G. Stress reduction using bilateral stimulation in virtual reality. IEEE Access. 2020; 8:200351-366. doi: 10.1109/ACCESS.2020.3035540 [Crossref]
- Vaghetti CAO, Botelho SSC. Virtual learning environments in physical education: a review of the use of exergames.
Ciênc Cogn. 2010;15(1):076-088. [cited 2024 July 5]. Available from:
http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1806-58212010000100008&lng=pt&nrm=iso
- Masroor S, Bhati P, Verma S, Khan M, Hussain ME. Heart Rate Variability following combined aerobic and resistance training in sedentary hypertensive women: a randomized control trial. Indian Heart J. 2018;28-35. doi: 10.1016/j.ihj.2018.03.005 [Crossref]
- Rodrigues RA, Ramos ACC, Santana MVB, Brasil CA, Dias CMCC, Macedo LB. Realidade virtual como recurso na reabilitação cardiovascular: revisão sistemática. ASSOBRAFIR Ciência. 2016;7(3):41-9. doi: 10.47066/2177-9333/AC.26553 [Crossref]